
30 Sep Diagnosing PCOS and PCOM
Polycystic ovary syndrome (PCOS) is the
most common endocrine disorder in women
of reproductive age and affects between 10%
and 21% of women depending on the diag–
nostic criteria used and population assessed.
The condition has many short-term and
long-term complications, including repro–
ductive (such as, amenorrhoea, anovulation,
hirsutism, infertility and pregnancy compli–
cations), metabolic (diabetes mellitus, dys–
lipidaemia and cardiovascular risk factors)
and psychological (depression, anxiety, body
image and quality of life) disorders.
PCOM is perhaps the most controversial
of the PCOS diagnostic criteria and is based
on the unilateral or bilateral presence of >12
follicles with a diameter of 2–9 mm and/or an
ovarian volume >10 ml. However, as
ultrasonography technology has advanced,
follicles are more easily detected than with
previous equipment, and the prevalence of
PCOM in the population is now between
20% in adults and 84% in adolescents with
current PCOM criteria, including many
without PCOS. Consequently, the Androgen
Excess and PCOS Society (AE–PCOS) task
force reviewed the evidence and published
recommendations in 2014 that aimed to
refine PCOM criteria and improve the accu-
racy of diagnosis of PCOS.
The task force recommended that PCOM
be defined as >25 follicles per ovary with
a diameter between 2 mm and 10 mm.
However, this definition was contingent on
the use of new ultrasonography technology
(with a transducer frequency >8 MHz). The
task force recognized that this technology is
not always available and ovarian volume of
>10 ml could be substituted as an alternative
for PCOM, which recognizes the limitations
in specificity and sensitivity compared with
follicle number per ovary.
However, no investigators have reported on the
adoption of these AE–PCOS recommendations
or described their practicality in clinical
care. Interestingly, the AE–PCOS task force
also reports that women with ‘mild’ PCOS
(hyperandrogenism plus PCOM (pheno–
type C) or oligo-ovulation or anovulation
plus PCOM (phenotype D)) would probably
have similar management and, therefore,
ultra sonography might not impact on clin–
ical care. Given these considerations and
the persisting need to still disseminate
and implement the AE–PCOS recommenda–
tions, their clinical relevance and impact are
difficult to judge.
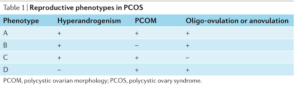
phenotype of PCOS
Source: Nature

